by The Children's Treatment Center | Mar 16, 2020 | General
We hope that you, your children and families are doing well in the midst of this unprecedented time. After carefully considering the CDC guidelines, we at The Children’s Center have decided that we will no longer be conducting therapy in our office at this time....

by The Children's Treatment Center | Feb 10, 2020 | General
We are all so “connected” nowadays. Everywhere you look, you see people of all ages engrossed in the online world. Children are asking for cellphones at younger and younger ages, while parents often seem so attached to their devices that they barely pay attention to...

by The Children's Treatment Center | Sep 18, 2019 | General
This summer’s hurricane season was fairly quiet until Hurricane Dorian blew through offshore earlier this month. Then, Humberto threatened the South Florida area last week, putting everyone on high alert for the second time in less than a month. For some children,...
by The Children's Treatment Center | Jul 29, 2019 | General
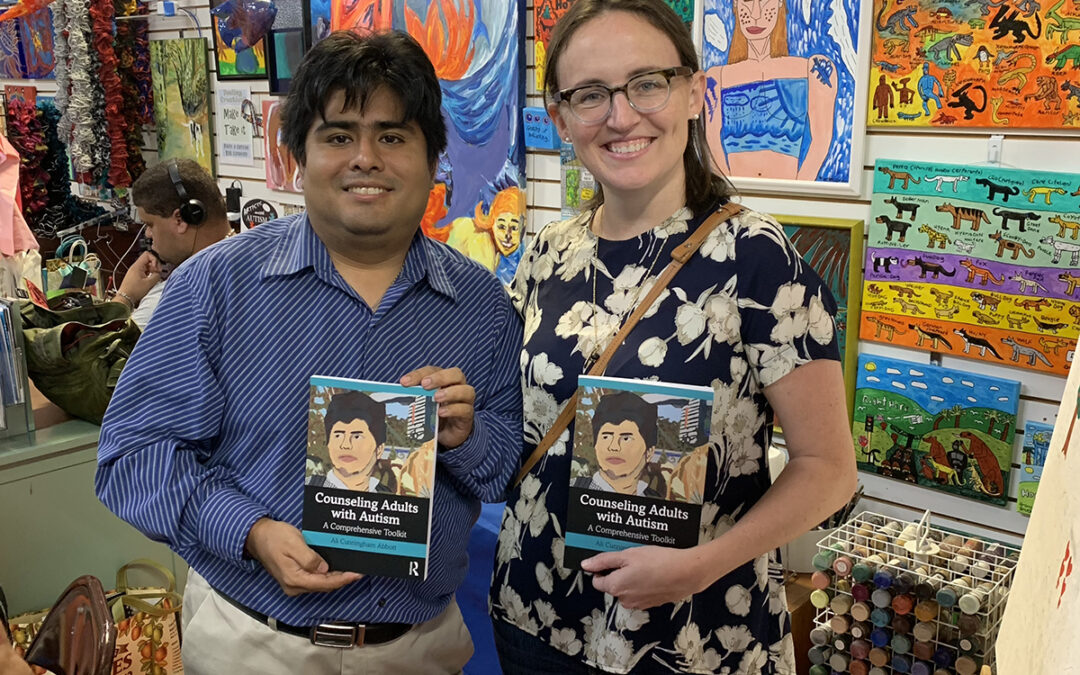
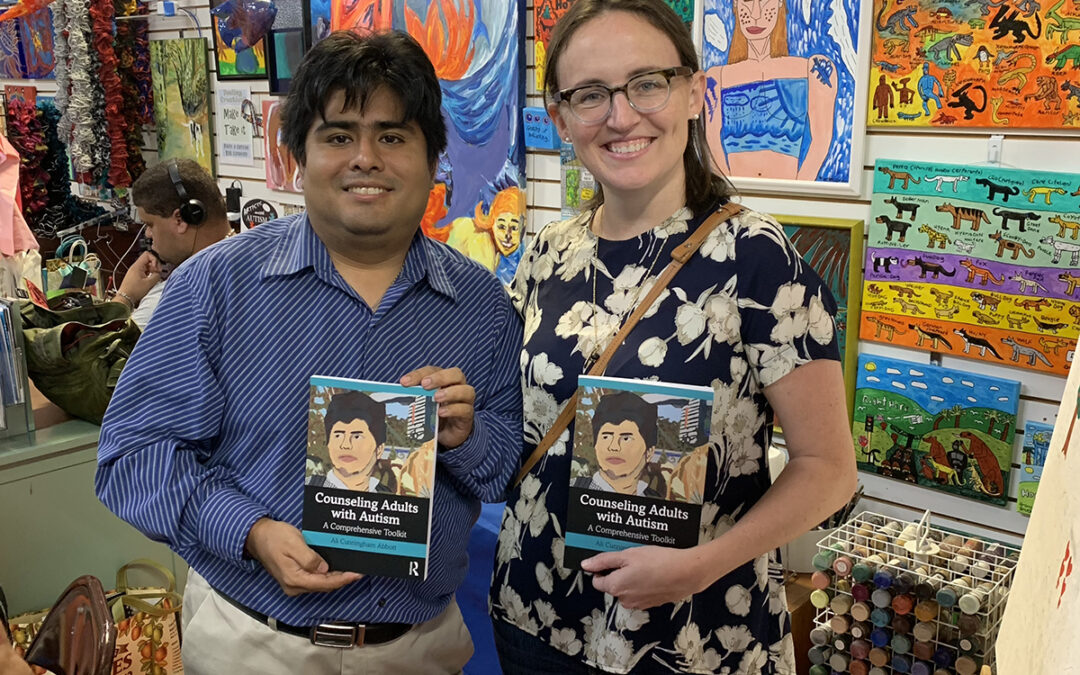
Our very own Dr. Ali Cunningham recently released a book, Counseling Adults with Autism. The cover art for the book was produced by a local man with autism, Michael Vidal (pictured here with Dr. Cunningham). Counseling Adults with Autism is a practical guide for...

by The Children's Treatment Center | Jul 12, 2019 | General
Toddlerhood is defined as the age range from 12 to 36 months. During this period, a child’s emotional and cognitive development grows by leaps and bounds, as do their social skills. This also coincides with the time when children are likely to go into a daycare...